Managing Your Flat Feet
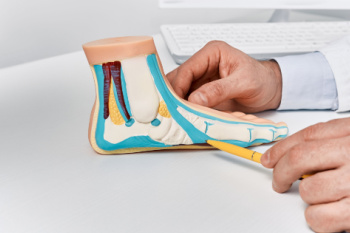
Flat feet, or fallen arches, occur when the arches of the feet collapse, causing the entire sole to touch the ground. While some individuals have flat feet from childhood, others may develop them later in life. A primary cause of flat feet is genetics. If your parents or grandparents had flat feet, there is a higher likelihood of inheriting the condition. Additionally, injuries or stress to the feet’s tendons and ligaments or standing for long periods of time can lead to flat feet. Symptoms may include foot pain, swelling, and difficulty with movement. In severe cases, surgical intervention may be necessary to reconstruct the arches. To accurately diagnose the extent of flat feet and determine what the most effective treatment plan is, it is important to consult a podiatrist. They can provide expert assessment, recommend appropriate interventions like custom orthotics, and ensure ongoing management to alleviate symptoms and improve foot function. It is suggested that you schedule an appointment with a podiatrist for personalized care and relief from flat feet.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Anthony Ricciardi Jr., DPM from Foot & Ankle Specialists of Nevada. Our Doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our office located in Las Vegas, Nevada . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Read more about What is Flexible Flat Foot?
What is Flexible Flat Foot?
Flatfoot is classified as having the entire sole of the foot in contact or near contact to the ground while standing. The disorder is also known as fallen arches, because those affected have no arch in their feet. Flexible flatfoot and rigid flatfoot are the two types of flatfoot.
A person has flexible flatfoot if when sitting or standing on their toes, they have an arch that disappears when they stand with the entire foot on the ground. Flexible flatfoot may also be called “pediatric flatfoot” because the condition first appears in childhood. It is common among infants because the arch does not develop until the age of 5 or 6 years. Rigid flatfoot is not as common in children as it is with adults. This type of flatfoot is developed due to the weakening of tibialis posterior muscle tendon, a major supporting structure of the foot arch. Development of this deformity is progressive and shows early signs of pain and swelling that begins at the inside arch of the foot and moves to the outside of the foot below the ankle. More severe cases can possibly lead to arthritis of the foot and ankle joints.
Although most cases of flatfoot involve people born with the condition, some less common causes are obesity, diabetes, pregnancy, and osteoporosis. In some cases, flatfoot may come with no symptoms at all and does not require any type of treatment. With other cases though, symptoms may include pain in the shin, knee, hips and lower back. If a person with flatfeet experiences such symptoms, a health care provider may suggest using orthotic devices or arch supports, which may reduce the pain. Wearing supportive shoes can also prove more comfortable with flatfeet and staying away from shoes with little support such as sandals. Other methods to relieve pain also include stretching the Achilles tendon properly and using proper form when doing any physical activity. In addition, losing weight can reduce the stress on your feet and reduce the pain.
Heel Pain in the Morning?

Heel pain can negatively affect your day-to-day life. Simple activities like walking can become incredibly uncomfortable or painful due to heel pain.
Don’t live with heel pain and get treated.
Managing an Ingrown Toenail

Onychocryptosis, commonly known as an ingrown toenail, occurs when the edge of a toenail grows into the surrounding skin, leading to pain, swelling, and sometimes infection. This condition often affects the big toe and can result from improper nail trimming, tight footwear, or injury to the toe. Managing an ingrown toenail involves several steps to alleviate discomfort and promote healing. Soaking the affected foot in warm water can soften the skin and reduce inflammation. Keeping the foot dry and wearing well-fitting shoes can prevent further irritation. Lifting the nail gently and placing a small piece of cotton or dental floss under it can help guide the nail to grow correctly. An ingrown toenail can cause significant pain and discomfort. If you have an ingrown toenail that has worsened, it is strongly suggested that you seek the advice of visit a podiatrist who can effectively treat this condition, which may include minor surgery.
Ingrown toenails can become painful if they are not treated properly. For more information about ingrown toenails, contact Anthony Ricciardi Jr., DPM of Foot & Ankle Specialists of Nevada. Our Doctor can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails occur when a toenail grows sideways into the bed of the nail, causing pain, swelling, and possibly infection.
Causes
- Bacterial infections
- Improper nail cutting such as cutting it too short or not straight across
- Trauma to the toe, such as stubbing, which causes the nail to grow back irregularly
- Ill-fitting shoes that bunch the toes too close together
- Genetic predisposition
Prevention
Because ingrown toenails are not something found outside of shoe-wearing cultures, going barefoot as often as possible will decrease the likeliness of developing ingrown toenails. Wearing proper fitting shoes and using proper cutting techniques will also help decrease your risk of developing ingrown toenails.
Treatment
Ingrown toenails are a very treatable foot condition. In minor cases, soaking the affected area in salt or antibacterial soaps will not only help with the ingrown nail itself, but also help prevent any infections from occurring. In more severe cases, surgery is an option. In either case, speaking to your podiatrist about this condition will help you get a better understanding of specific treatment options that are right for you.
If you have any questions please feel free to contact our office located in Las Vegas, Nevada . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Read more about Ingrown Toenails
Ingrown Toenails
An ingrown toenail is a nail that has curved downward and grown into the skin. This typically occurs at either the nail borders or the sides of the nail. As a result, pain, redness, swelling, and warmth may occur in the toe. If a break in the skin forms due to the ingrown nail, bacteria may enter and cause an infection in the area; this is typically characterized by a foul odor and drainage.
Ingrown toenails have multiple reasons for developing. In many instances, the condition is a result of genetics and is inherited. The most common cause, however, is improper trimming; cutting the toenails too short forces the skin beside the nail to fold over. An ingrown toenail can also develop due to trauma, such as stubbing the toe, having an object fall on the toe, or participating in activities that involve repeated kicking or running. Wearing shoes that are too tight or too short can also cause ingrown toenails.
Treatment for an ingrown toenail varies between patients and the severity of the condition. In most cases, it is best to see your podiatrist for thorough and proper treatment. After examining your toe, your podiatrist may prescribe oral antibiotics to clear the infection if one is present. Surgical removal of either a portion of the nail or the entire nail may also be considered. In some cases, complete removal or destruction of the nail root may be required. Most patients who undergo nail surgery experience minimal pain afterward and can return to normal activity the following day.
Ingrown toenails can be prevented with proper nail trimming and by avoiding improper-fitting shoes. When cutting the toenails, be sure that you are cutting in a straight line and avoid cutting them too short. Shoes should not be too short or tight in the toe box.
Causes of Foot and Ankle Injuries in Dancers
 Dancers are prone to foot and ankle injuries due to the physical demands of their art. Risk factors can include inadequate warm-up, improper technique, and wearing unsuitable footwear. Overuse injuries, such as tendinitis and stress fractures, result from repetitive movements and intense training schedules. Acute injuries often occur from sudden movements or missteps, leading to sprains or fractures. Additionally, common ankle injuries in dancers include lateral ankle sprains, where the ligaments on the outside of the ankle are stretched or torn, and Achilles tendinitis, which causes pain and inflammation in the tendon connecting the calf muscle to the heel. Ensuring proper warm-up routines, using supportive footwear, and focusing on technique can help prevent these injuries. Regular strength and flexibility training also play a critical role in maintaining foot and ankle health for dancers. If you are engaged in any type of dance and have endured a foot or ankle injury, it is suggested that you visit a podiatrist who can offer effective treatment methods.
Dancers are prone to foot and ankle injuries due to the physical demands of their art. Risk factors can include inadequate warm-up, improper technique, and wearing unsuitable footwear. Overuse injuries, such as tendinitis and stress fractures, result from repetitive movements and intense training schedules. Acute injuries often occur from sudden movements or missteps, leading to sprains or fractures. Additionally, common ankle injuries in dancers include lateral ankle sprains, where the ligaments on the outside of the ankle are stretched or torn, and Achilles tendinitis, which causes pain and inflammation in the tendon connecting the calf muscle to the heel. Ensuring proper warm-up routines, using supportive footwear, and focusing on technique can help prevent these injuries. Regular strength and flexibility training also play a critical role in maintaining foot and ankle health for dancers. If you are engaged in any type of dance and have endured a foot or ankle injury, it is suggested that you visit a podiatrist who can offer effective treatment methods.
Ankle and foot injuries are common among athletes and in many sports. They can be caused by several problems and may be potentially serious. If you are feeling pain or think you were injured in a sporting event or when exercising, consult with Anthony Ricciardi Jr., DPM from Foot & Ankle Specialists of Nevada. Our Doctor will assess your condition and provide you with quality foot and ankle treatment.
Common Injuries
The most common injuries that occur in sporting activities include:
- Achilles Tendonitis
- Achilles Tendon Rupture
- Ankle Sprains
- Broken Foot
- Plantar Fasciitis
- Stress Fractures
- Turf Toe
Symptoms
Symptoms vary depending upon the injury and in some cases, there may be no symptoms at all. However, in most cases, some form of symptom is experienced. Pain, aching, burning, bruising, tenderness, tightness or stiffness, sensation loss, difficulty moving, and swelling are the most common symptoms.
Treatment
Just as symptoms vary depending upon the injury, so do treatment options. A common treatment method is known as the RICE method. This method involves rest, applying ice, compression and elevating the afflicted foot or ankle. If the injury appears to be more serious, surgery might be required, such as arthroscopic or reconstructive surgery. Lastly, rehabilitation or therapy might be needed to gain full functionality in the afflicted area. Any discomfort experienced by an athlete must be evaluated by a licensed, reputable medical professional.
If you have any questions, please feel free to contact our office located in Las Vegas, Nevada . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Read more about Sports Related Foot and Ankle Injuries
Sports Related Foot and Ankle Injuries
Foot and ankle injuries are common among athletes and those who exercise frequently. Most of these injuries are non-life-threatening and can heal in weeks with proper treatment and care. Serious injuries, however, require urgent medical treatment.
Common minor injuries include ankle sprains, ankle strains, Achilles tendonitis, plantar fasciitis, stress fractures, and turf toe. An ankle sprain is when the ligaments in the ankle have either become stretched or torn. When the muscle or tendon is stretched or torn, it is an ankle strain. When the big toe is sprained, it is known as turf toe. Achilles tendonitis is the overuse and inflammation of the Achilles tendon. Plantar fasciitis is the inflammation of the plantar fascia and generally occurs from overuse in athletics. Stress fractures are also caused from overuse and are small cracks in the bone.
Achilles tendon ruptures are common, but more serious. This injury occurs when the Achilles tendon, the largest tendon in the body, ruptures. In most cases, this causes severe pain and difficulty walking; some who have experienced this injury have reported, however, no signs or symptoms. A laceration is a deep cut that can occur anywhere on the body. Lacerations on the foot are rarer, but can occur from things like metal cleats landing on the foot.
Treatment options cover a wide range of methods based upon the injury and its severity. Conditions like plantar fasciitis, stress fractures, Achilles tendonitis, turf toe and ankle sprains/ strains can heal on their own without immediate medical care, but seeing a podiatrist to monitor the injury is always recommended. Following the RICE (Rest, Icing, Compression, and Elevation) protocol is generally enough to treat minor injuries. This means resting the foot by either keeping pressure off the foot or not walking at all. Icing the injury will help reduce swelling and pain. Compressing the wound with a wrap will immobilize and help promote healing. Finally, keeping the wound elevated will also reduce swelling and also help the healing process.
It is important to note that even minor injuries can vary in severity, with grade one being a minor injury and grade three requiring urgent care by a podiatrist. Achilles tendon ruptures and lacerations on the foot generally require urgent medical care and treatment options that need a podiatrist. These could include imaging tests, stitches for cuts, rehabilitation, and casts or braces. Every case is different, however, so it is always recommended to see a podiatrist when pain in the foot does not disappear.
What to Do About Gout
 Gout is a type of arthritis caused by the accumulation of uric acid crystals in the joints, often affecting the feet, particularly the big toe. It leads to sudden, severe pain, in addition to redness and swelling. Gout predominantly affects middle-aged men and postmenopausal women, especially those with a diet high in purines, a substance found in red meat and alcohol. The condition is often diagnosed through blood tests measuring uric acid levels and joint fluid analysis to detect urate crystals. Treatment focuses on reducing pain and inflammation with nonsteroidal anti-inflammatory drugs, corticosteroids, or colchicine. Long-term management includes medications like allopurinol or febuxostat to lower uric acid levels. For foot-specific care, patients may elevate the affected foot and wear comfortable, supportive footwear to alleviate symptoms and prevent flare-ups. Preventing gout involves maintaining a healthy diet, staying hydrated, and avoiding foods high in purines. Regular exercise and weight management are also critical. If you have gout that is negatively impacting your feet, it is suggested that you consult a podiatrist for specialized care and tailored advice.
Gout is a type of arthritis caused by the accumulation of uric acid crystals in the joints, often affecting the feet, particularly the big toe. It leads to sudden, severe pain, in addition to redness and swelling. Gout predominantly affects middle-aged men and postmenopausal women, especially those with a diet high in purines, a substance found in red meat and alcohol. The condition is often diagnosed through blood tests measuring uric acid levels and joint fluid analysis to detect urate crystals. Treatment focuses on reducing pain and inflammation with nonsteroidal anti-inflammatory drugs, corticosteroids, or colchicine. Long-term management includes medications like allopurinol or febuxostat to lower uric acid levels. For foot-specific care, patients may elevate the affected foot and wear comfortable, supportive footwear to alleviate symptoms and prevent flare-ups. Preventing gout involves maintaining a healthy diet, staying hydrated, and avoiding foods high in purines. Regular exercise and weight management are also critical. If you have gout that is negatively impacting your feet, it is suggested that you consult a podiatrist for specialized care and tailored advice.
Gout is a foot condition that requires certain treatment and care. If you are seeking treatment, contact Anthony Ricciardi Jr., DPM from Foot & Ankle Specialists of Nevada. Our Doctor will treat your foot and ankle needs.
What Is Gout?
Gout is a type of arthritis caused by a buildup of uric acid in the bloodstream. It often develops in the foot, especially the big toe area, although it can manifest in other parts of the body as well. Gout can make walking and standing very painful and is especially common in diabetics and the obese.
People typically get gout because of a poor diet. Genetic predisposition is also a factor. The children of parents who have had gout frequently have a chance of developing it themselves.
Gout can easily be identified by redness and inflammation of the big toe and the surrounding areas of the foot. Other symptoms include extreme fatigue, joint pain, and running high fevers. Sometimes corticosteroid drugs can be prescribed to treat gout, but the best way to combat this disease is to get more exercise and eat a better diet.
If you have any questions please feel free to contact our office located in Las Vegas, Nevada . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Read more about Everything You Need to Know About Gout
Everything You Need to Know About Gout
Gout, typically found in diabetic patients, is an unusually painful form of arthritis caused by elevated levels of uric acid in the bloodstream. The condition typically strikes the big joint on the big toe. It has also been known to strike the knees, elbows, fingers, ankles and wrists—generally anywhere that has a functioning, moving joint.
The high level of uric acid in a person’s bloodstream creates the condition known as hyperuricema—the main cause of gout. Genetic predisposition occurs in nine out of ten sufferers. The children of parents who suffer gout will have a two in ten chance of developing the condition as well.
This form of arthritis, being particularly painful, is the leftover uric acid crystallizing in the blood stream. The crystallized uric acid then travels to the space between joints where they rub, causing friction when the patient moves. Symptoms include: pain, redness, swelling, and inflammation. Additional side effects may include fatigue and fever, although reports of these effects are very rare. Some patients have reported that pain may intensify when the temperature drops, such as when you sleep.
Most cases of gout are easily diagnosed by a podiatrist’s assessment of the various symptoms. Defined tests can also be performed. A blood test to detect elevated levels of uric acid is often used as well as an x-ray to diagnose visible and chronic gout.
Treatment for gout simply means eliminating symptoms. Non-steroid anti-inflammatory drugs or NSAIDs (Colchicine and other corticosteroid drugs, etc.) will quell the redness, the swelling, and the inflammation. However, managing your diet, lifestyle changes, and using preventative drugs are all helpful toward fully combating the most severe cases.
Those that lead an inactive lifestyle are at a higher risk for gout. Any amount of exercise decreases the probability of repeat encounters with the condition. Reducing your consumption of red meat, sea food, and fructose-sweetened drinks also reduces the likelihood of chronic gout as well.
Ingesting Vitamin C, coffee, and particular dairy products can help with maintaining a healthy lifestyle. There are new drugs out on the market that inhibit the body’s production of uric acid-producing enzymes. However, reducing or eliminating your overall levels of uric acid is the best remedy to ensuring you lead a gout-free life.
Exploring the Causes of Foot and Ankle Pain

Foot and ankle pain can stem from a variety of sources, each with its unique challenges. Bruises often result from direct trauma, causing discoloration and tenderness. Puncture wounds, which may occur from stepping on sharp objects, can lead to infection if not properly treated. Injuries to ligaments and tendons, such as sprains and strains, are common, and typically result from overuse or sudden twists and turns, leading to swelling and pain. Dislocations, though less frequent, can occur from severe trauma, necessitating medical intervention to realign the bones. Retrocalcaneal bursitis, an inflammation of the bursa located at the back of the heel, often arises from repetitive stress or ill-fitting shoes, causing pain and swelling near the Achilles tendon. Addressing foot and ankle pain effectively requires identifying the specific cause and implementing appropriate treatments. If you have any type of foot or ankle pain, it is suggested that you are under the care of a podiatrist who can offer you effective treatment options.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Anthony Ricciardi Jr., DPM from Foot & Ankle Specialists of Nevada. Our Doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our office located in Las Vegas, Nevada . We offer the newest diagnostic and treatment technologies for all your foot care needs.
